I feel strange... Something just does not feel right. I'm starting to feel kinda happy. I think I like it! Wait a sec... I am flying west of Aspen, Colorado at 16,500’ MSL in a Cirrus SR-22TN and I am using Supplemental O2. I think maybe I might be suffering from Hypoxic Hypoxia. I think I remember learning about this during my Private Pilot training. My instructor told me that Aeromedical Factors was critical to safe operation of my airplane and perhaps even my own survival in an emergency.
At 16,500’ MSL while flying over the rockies on your way to Las Vegas, Nevada. You are flying in hard IMC at night, in IFR conditions. You’re using Supplemental O2, but you just don’t feel right. You realize that you are definitely starting to feel the effects of Hypoxic Hypoxia. You know this because you recently just finished reviewing Aeromedical Factors and were able to quickly identify the symptoms of Hypoxia. Realizing there is a problem with the O2 System, you begin an Emergency Descent to a lower altitude, then land; saving the day!
The objective of the Aeromedical Factors lesson is to explain the effects and/or various factors that affect the body while inflight and how to recognize and properly manage these events.
Aeromedical Factors is a very important lesson that should be taught in-depth to every student that a CFI works with. The fundamentals of Aeromedical Factors need to establish the seriousness and inherent dangers that exist in-flight and how to properly apply this knowledge to combat a potential aviation incident or accident. In General Aviation's history, it has been proven that a significant number of accidents could have been prevented if the pilot had a solid understanding of Aeromedical Factors.
As an Aviation Instructor (CFI) it is your top priority to be teaching at every opportunity each every student as in-depth as possible about this lesson. Use NTSB Investigation Reports that cover past aviation incidents, use images, use different perspectives. If your student has questions that you don't have answers to. Take the time to do the research, see what you yourself can learn by that research.
Your student's perception is their reality. As a CFI, you are viewed as the gateway to aviation. The source of all knowledge. But remember, you're not perfect and you don't know everything. Take the time to do research and work with your students to educate them on everything Aeromedical Factors!
Each airman exercising the privileges of flight (excluding a CFI who is providing instruction to an already certificated pilot) must hold some type of Medical Certificate.
Obtaining a Medical Certificate is serious business. Being DENIED for a Medical Certificate is a potentially life-impacting event. Before encouraging a student to “Go Get the Medical” a caring and courteous instructor will have a discussion with the applicant to ensure that they do not have any major roadblocks, which could potentially prevent the student from obtaining the Medical Certificate.
Find an AME to obtain a Medical Certificate by visiting the FAA website.
Visit the FAA MedExpress Website to apply for the Medical Certificate.
Having a medical problem is not always a GAME OVER event. In certain cases, it may be possible to obtain a Statement of Demonstrated Ability (SODA) Waiver. This waiver may be granted to a person who does not meet the applicable standards of FAR Part 67. The SODA can be withdrawn, at the discretion of the Federal Air Surgeon, at any time.
A Flight Instructor does not need a Medical Certificate to provide instruction to a student, provided the instructor is NOT acting a Pilot-In-Command of the aircraft. An example would be providing a Private Pilot with CFII Instruction.
A CFI needs a minimum of a 3rd Class Medical Certificate to act as Pilot-In-Command.
A Light Sport Aircraft Pilot (LSA) does NOT need a Medical Certificate. A Driver License (DL) is used in lieu of a Medical Certificate.
If an applicant was recently denied for a Medical Certificate. They cannot fly under FAA BasicMed, nor can they use their Driver License in lieu of the medical for a Sport Pilot Certificate.
Code of Federal Regulations (FAR §67) - This part prescribes the medical standards and certification procedures for issuing medical certificates for airmen and for remaining eligible for a medical certificate.
There are several different types of traditional Medical Certificates that are issued based on the type of flying privileges the pilot will exercise. Typically, a Student Pilot will obtain a Third Class Certificate from an AME to be afforded Solo privileges, thence Private Pilot Privileges (once the practical has been passed).
It’s important to remember that when an FAA Medical Certificate expires. The certificate never changes. The only thing that changes are the privileges which are allowed to be exercised. Reference FAR Part §61.23 for more details.
Code of Federal Regulations (FAR §61.23) - This specific regulation covers Medical Certificates, their requirements and duration. It also covers operations which do not require a Medical Certificate.
FAA Third Class Medical Reform was signed into law on July 15, 2016. On January 10, 2017 the FAA published a final rule, based on the legislation, setting May 1 as the effective date. FAA BasicMed was born.
You must have previously been issued an FAA Medical Certificate from an authorized AME. Even if it has expired (assuming that it has not lapsed more than 10 years before July 15, 2016).
Pilots whose most recent medical certificate has been revoked, suspended, or withdrawn, had his or her most recent application denied, or authorization for special issuance withdrawn, will need to obtain a new medical certificate before they can operate under BasicMed.
FAA Basic Med allows pilots flying under the new rules to operate “covered aircraft” defined as having MGTOW of not more than 6,000 pounds and are authorized to carry not more than 6 occupants which are operated while carrying up to five passengers in addition to the pilot in command, at altitudes up to 18,000 feet MSL and at an airspeed of up to 250 KIAS.
Pilots, if appropriately rated, can fly VFR or IFR in said “covered aircraft.” Pilots flying under the exemption cannot operate for compensation or hire, and must operate within the United States, unless authorized by the country in which the flight will be conducted.
Once every four years (48 months), the pilot needs to visit a state-licensed physician who will affirm that a health examination has been performed, and that the applicant is still fit to fly.
An FAA checklist will be filled out by the doctor. This form must be retained with the pilot’s logbook (paper or electronic). It would only need to be provided to the FAA upon request (such as a ramp check, investigation, or enforcement action).
Every two years (24 calendar months), the pilot will also need to take the free AOPA Medical Self Assessment Course.
First thing's first. What does IACRA stand for? Integrated Airman Certification and Rating Application (IACRA). What does it do? IACRA is a web-based certification/rating application website that our friends at the FAA use to help guide an applicant through the process of obtaining a certificate.
First, an applicant submits an application for a certificate or rating. After the applicant takes the test, the applicant provides their FAA Tracking Number (FTN) to their instructor, Designated Pilot Examiner (DPE), Aircrew Program Designee (APD), or FAA Inspector who will later certify the application after a pass or fail event and gives the capability to print a temporary certificate.
An authorized Flight Instructor, DPE, or Airman Certification Representative at a Part 141 flight school must process an application with a student for a Student Pilot Certificate through IACRA.
As a part 61 flight instructor, you will be responsible for obtaining the Student Pilot Certificate for your student, unless there is a dedicated representative at your school who completes them for you.
The Student Pilot Certificate may also be requested in paper format, by using FAA form 8710-1. If the form is completed by paper, it should be submitted to the nearest FSDO where the student will be completing his or her flight training.
Once, reviewed by the Airman Certification Branch, the student pilot certificate will be mailed to the address provided by the applicant. The Student Pilot Certificate will take approximately one month to be received by the applicant. The applicant will receive a plastic Student Pilot Certificate.
For Instructions on how to complete the IACRA. Please see the IACRA New User Guide for Student Pilots on the FAA's website.
Additionally, the applicant may use the document found here as a supplemental resource for applying to get a Student Pilot Certificate.
Solo endorsements are now placed in the student logbook and are no longer required to be on the student pilot certificate. Any previous endorsements on a paper student pilot certificate should be maintained as part of the required training record. For more information on the changes issued February 25, 2016. Please review the article on the AOPA Website titled "Working With The New Student Pilot Rules."
The brain relies on oxygen to carry out even the most fundamental functions, and without it, the brain rapidly ceases to operate. Prolonged oxygen deprivation can lead to death or permanent brain damage. Hypoxia, in essence, is the deprivation of oxygen to the brain, affecting blood, cells, and tissue.
Now, let's delve into the various types of hypoxia and their implications for aviation safety.
Hypoxic Hypoxia occurs at the lung level and is a result of insufficient oxygen. It is caused by reduced air pressure, typically encountered at higher altitudes. This form of hypoxia is the most common and is often associated with an aircraft depressurization event at high altitudes.
Hypemic Hypoxia results from the blood's incapacity to effectively transport oxygen. This condition arises when the blood fails to absorb and transport oxygen to the body's cells. Hypemic Hypoxia is frequently associated with some form of bodily impairment, with Carbon Monoxide (CO) poisoning being the most common cause.
Stagnant Hypoxia occurs due to poor blood circulation, resulting from inadequate blood flow to the bodily extremities. This form of hypoxia may manifest when the body is exposed to cold temperatures for an extended period. Instances include scenarios like rapid aircraft depressurization during flight or operating an aircraft in cold weather conditions without cabin heating.
Histotoxic Hypoxia is a condition that manifests at the cellular level, wherein the body encounters difficulty utilizing oxygen to support cellular metabolism. In this type of hypoxia, although oxygen may be present in the bloodstream, the cells themselves are unable to effectively utilize it. Histotoxic Hypoxia is often associated with factors such as alcohol consumption, poisoning, or pharmacological impairments.
This condition underscores the crucial role of cellular function in oxygen utilization. When impaired, even if the blood carries sufficient oxygen, the body's cells are unable to extract and use it efficiently. Recognizing the potential causes, such as alcohol consumption or exposure to toxins, is paramount for pilots to take preventive measures and maintain optimal physiological conditions during flight. Awareness and proactive steps to mitigate the risk of Histotoxic Hypoxia are essential components of aviation safety protocols.
Fulminating Hypoxia is a critical condition that arises when oxygen is swiftly expelled from the lungs, often associated with a rapid depressurization of an aircraft at high altitude. This type of hypoxia is not only intensely painful but can also inflict physical damage on the lungs. In the event of Fulminating Hypoxia due to sudden depressurization, a pilot's time of useful consciousness is dramatically reduced, effectively halving the window for making life-saving decisions.
The urgency of response in such situations cannot be overstated, and pilots must act swiftly to deploy supplemental oxygen, initiate an emergency descent, and promptly communicate the emergency to air traffic control. The brief and critical nature of this condition underscores the importance of rigorous training and preparedness to enhance a pilot's ability to manage and navigate through this potentially life-threatening scenario.
Hypoxia often reveals itself through a series of distinctive signs and symptoms:
Feelings of Carelessness and Euphoria: Initial stages may manifest as a sense of carelessness and euphoria. Interestingly, this sensation can be simulated in the aircraft by subjecting it to increased positive load factors, essentially pulling some G's.
Cyanosis: A noticeable indication of advanced hypoxia is cyanosis, characterized by a bluish tint in the fingernails and lips. This may be accompanied by a headache.
Decreased Reaction Times: Hypoxia can result in reduced reaction times, affecting a pilot's ability to respond quickly and effectively.
Impaired Judgement and Decision-Making Abilities: Judgement and decision-making abilities may become compromised, leading to potentially dangerous situations.
Visual Impairment: Hypoxia can cause visual disturbances, impacting a pilot's ability to perceive and interpret information accurately.
Drowsiness: A sense of drowsiness may set in, further hampering alertness and cognitive function.
Lightheadedness or Dizziness: Hypoxia often induces lightheadedness or a dizzy sensation, which can contribute to disorientation.
Tingling Extremities: Hypoxia may result in tingling sensations in the extremities, particularly in the fingers or toes, which can progress to numbness.
Recognizing these symptoms promptly is crucial for pilots to take immediate corrective action, such as descending to a lower altitude, using supplemental oxygen, and declaring an emergency if necessary. Regular training and awareness are essential for mitigating the risks associated with hypoxia during flight.
This video highlights the Air Force's pilot training on recognizing and managing Hypoxia during cabin pressure loss scenarios. It blends theory and simulations to enhance pilots' decision-making in high-altitude flight, prioritizing safety for both pilots and aircraft.
The ease or difficulty of treating hypoxia depends on its type, and in professional aviation, the most common hypoxia encountered by pilots is associated with a lack of air pressure, known as Hypoxic Hypoxia. However, in general aviation, particularly in single-engine piston aircraft during colder months, another type, Hypemic Hypoxia, may be a reality due to the exhaust manifold being utilized for the cabin heating system.
For Hypoxic Hypoxia, the recommended treatment involves descending the aircraft to a lower altitude and using supplemental oxygen if available.
In the case of Hypemic Hypoxia, immediate actions include shutting off the cabin heating system, opening all available sources of air ventilation such as windows and vents, and using supplemental oxygen if accessible. It is crucial to declare an emergency and land the aircraft as soon as possible.
Fulminating Hypoxia demands swift action. Immediate use of supplemental oxygen delivered to the lungs under positive pressure is required, followed by an emergency descent. An emergency declaration should be made to air traffic control (ATC).
For the remaining types of hypoxia, in-flight treatment is impossible. If any of these types are experienced, the recommended steps include using supplemental oxygen if available, declaring an emergency if possible, and landing the aircraft as soon as practicable. These measures underscore the critical importance of prompt and decisive actions to ensure the safety of both the pilot and the aircraft.
At higher altitudes, the reduction in air pressure poses challenges to breathing. Although the volume of air remains constant, the decreased atmospheric pressure makes it more difficult for your body to extract the necessary oxygen from that volume.
Gravity on Earth causes the breathable atmosphere to concentrate closer to the ground, primarily below 10,000 feet MSL (Mean Sea Level). Consequently, at higher altitudes or elevated Cabin Pressure Altitudes, breathing becomes challenging and, in extreme cases, impossible without the aid of supplemental oxygen delivered to the lungs under positive pressure.
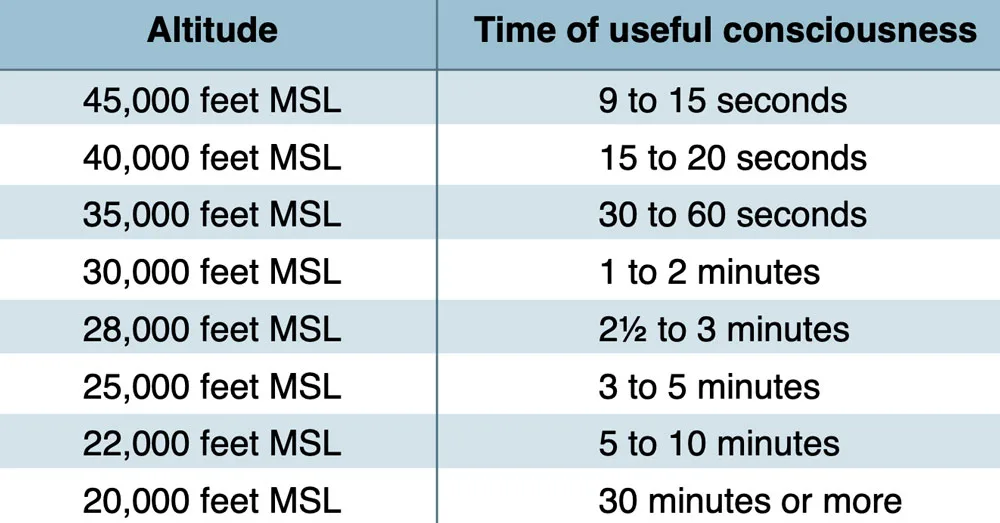
The video vividly illustrates how cognitive function experiences a rapid decline mere seconds after an increase in cabin altitude, leading to oxygen deprivation in the brain. This phenomenon is a clear manifestation of "time of useful consciousness," which can be succinctly defined as the duration during which a pilot remains cognitively coherent enough to perform tasks requiring high-level brain function.
In the event of a cabin depressurization incident, swift action is paramount. Pilots, especially those operating transport category aircraft, must promptly don an oxygen mask. The time of useful consciousness in such scenarios can be incredibly brief, measured in mere seconds, underscoring the critical importance of immediate response to ensure safety and the ability to execute necessary tasks.
During hypobaric chamber or altitude chamber training, individual #14 exhibited symptoms of hypoxia. It was observed that these symptoms became apparent after surpassing his time of useful consciousness (TUC). This underscores the critical importance of recognizing and addressing hypoxia promptly, especially in simulated high-altitude conditions. The incident highlights the need for effective training to ensure pilots and individuals in similar scenarios can identify symptoms, manage hypoxia, and take timely corrective actions to maintain safety and optimal cognitive function.
Hyperventilation is a condition characterized by rapid and excessive breathing. Healthy respiration involves a delicate equilibrium between inhaling oxygen and exhaling carbon dioxide. However, this equilibrium falters during hyperventilation, as the exhalation surpasses inhalation, resulting in a swift decrease in carbon dioxide levels within the body.
By definition, hyperventilation signifies an abnormal depletion of carbon dioxide (CO2) in the bloodstream. Insufficient levels of carbon dioxide prompt the constriction of blood vessels supplying the brain. This diminished blood supply to the brain manifests in symptoms such as light-headedness and tingling sensations in the fingers. In severe cases, hyperventilation can progress to a loss of consciousness.
Visual Impairment: Blurred vision or difficulty focusing may occur as a result of the altered respiratory pattern associated with hyperventilation.
Unconsciousness: In severe cases, hyperventilation can lead to a loss of consciousness. This underscores the critical importance of addressing hyperventilation promptly.
Lightheaded or Dizzy Sensation: A feeling of lightheadedness or dizziness is a common symptom, reflecting the impact of rapid breathing on the body's oxygen and carbon dioxide balance.
Tingling Sensations or Numbness: Hyperventilation can lead to changes in blood chemistry, resulting in tingling sensations or numbness, especially in the extremities.
Hot and Cold Sensations: Individuals experiencing hyperventilation may report sensations of feeling excessively hot or cold. These temperature fluctuations can be a response to the physiological changes induced by rapid breathing.
Muscle Spasms: Hyperventilation may contribute to muscle spasms, which can range from mild discomfort to more pronounced contractions.
Recognizing and addressing these symptoms promptly is crucial to managing hyperventilation effectively. Techniques such as controlled breathing and creating a more relaxed breathing pattern can help restore the balance of oxygen and carbon dioxide in the body.
Acute cases of hyperventilation can be effectively addressed by focusing on increasing carbon dioxide levels in the body, thereby slowing down the breathing rate. Here are some techniques:
Breathe Slowly Into a Paper Bag or Cupped Hands:
Inhale and exhale slowly into a paper bag or cupped hands. This helps to re-inhale some of the exhaled carbon dioxide, promoting a more balanced level in the body.
Talking Aloud as You Would in Conversation with Another:
Engage in verbal communication at a normal conversational pace. This encourages a more controlled and regular breathing pattern, assisting in the restoration of a proper balance of gases in the respiratory system.
Hold Your Breath for 10 to 15 Seconds at a Time:
Periodically hold your breath for short intervals, such as 10 to 15 seconds. This can contribute to the retention of carbon dioxide and aid in stabilizing the breathing rate.
It's important to note that these techniques should be practiced cautiously and under appropriate circumstances. If hyperventilation persists or is severe, seeking medical attention is advisable. Additionally, focusing on long-term strategies to manage stress and anxiety can be beneficial in preventing recurrent episodes of hyperventilation.
Aviators heavily rely on three crucial systems for maintaining postural control and balance: the Visual System, the Vestibular System, and the Somatosensory System. These systems provide sensory information that must be effectively regulated by the Central Nervous System (CNS).
The integration and coordination of inputs from these systems are vital for pilots to navigate and respond appropriately to the dynamic and often challenging conditions experienced during flight. A well-regulated interplay between the Visual, Vestibular, and Somatosensory Systems is essential for ensuring optimal spatial orientation and equilibrium in aviation contexts.
The Visual System holds significant importance in aviation, contributing to approximately ninety percent of the information used for establishing a point of reference. It plays a crucial role in resolving conflicting sensations from other sensory systems, enabling us to perform tasks with normalcy. Vision is instrumental in maintaining the proper orientation of the aircraft to Earth by referencing the ground, sky, and horizon.
While vision is generally reliable, it is not immune to illusions. These illusions can lead to errors in processing or interpreting visual cues, ultimately resulting in spatial disorientation. Pilots must be aware of these potential pitfalls, diligently cross-referencing visual information with inputs from other sensory systems, and staying vigilant to mitigate the risk of spatial disorientation during flight.
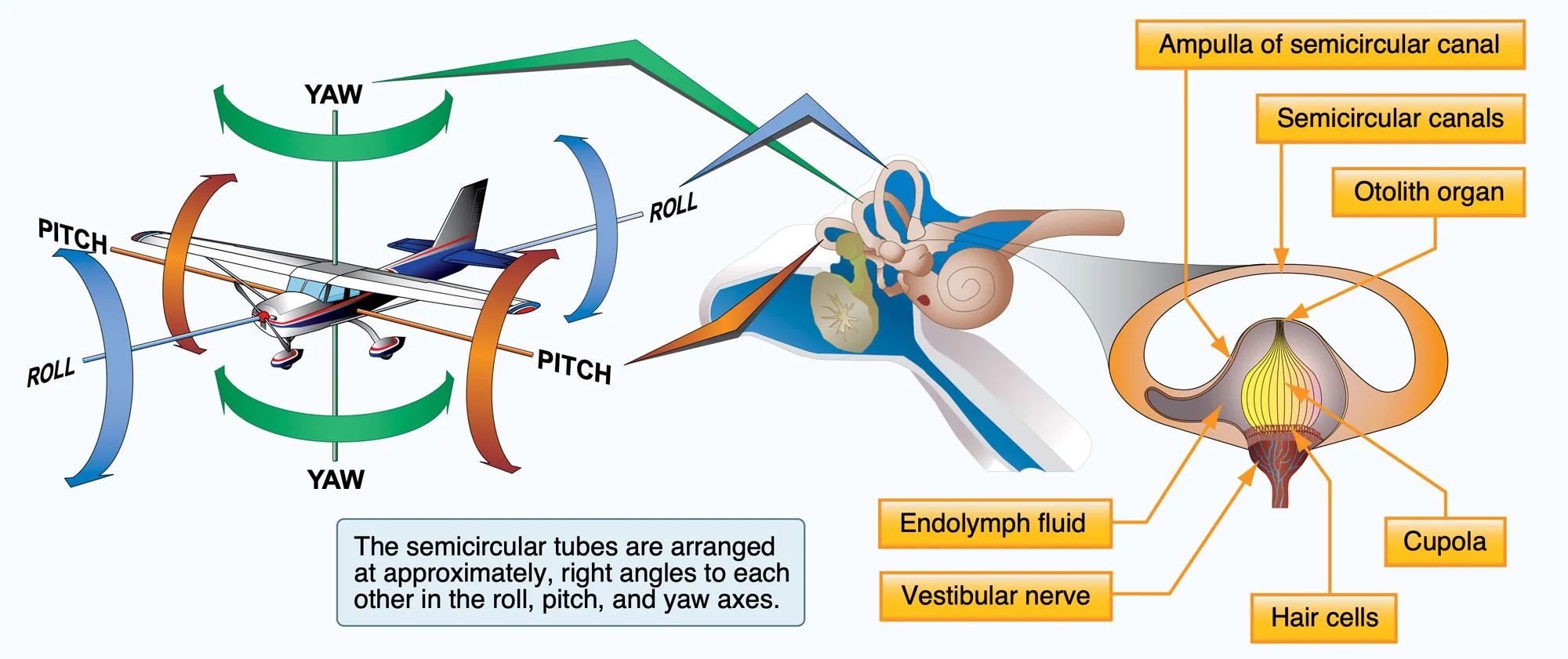
The Vestibular System is instrumental in enabling pilots to sense movement, referred to as the kinesthetic sense. This system serves as the primary means by which humans perceive balance and spatial orientation, facilitating the coordination of movement with balance. Within the inner ear's membranous labyrinth, the Vestibular System comprises three semicircular ducts (horizontal, anterior, and posterior), two otolith organs (saccule and utricle), and the cochlea. This complex structure allows pilots to maintain a keen awareness of their body's position and movement, contributing significantly to the precision and coordination required during flight activities.
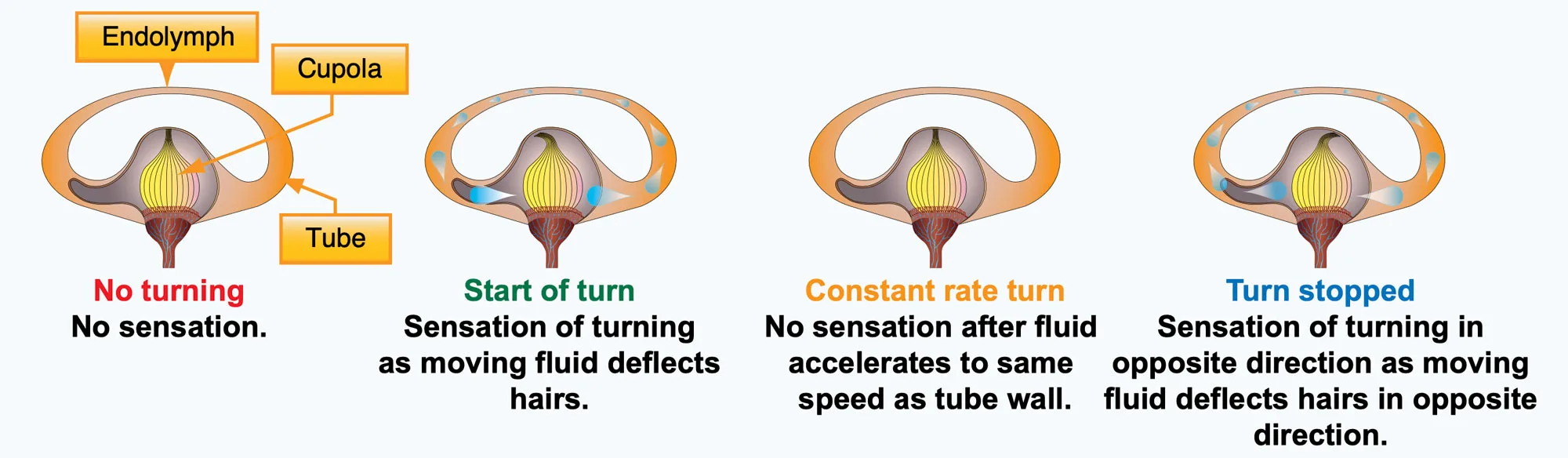
The semicircular canals are specialized structures that respond to angular acceleration, crucial for detecting rotational movement. Filled with Endolymph fluid, these canals play a pivotal role in our vestibular system. When the head changes position, the fluid in the canals lags behind due to inertia. This lagging motion acts on the Cupula, a gelatinous structure, causing it to bend the cilia of the hair cells. These hair cells, in turn, serve as sensory receptors, enabling the perception of movement.
It's worth noting that within the Semicircular Canals, we also find the Otolith Organs, which include the saccule and utricle. Together, these components of the Vestibular System contribute to our ability to sense and respond to changes in position and movement, playing a crucial role in maintaining balance and spatial orientation, particularly for pilots during flight.
The Somatosensory System, also known as the proprioceptive system, is integral to our ability to perceive the body's position and movement. Proprioception involves adjusting muscle contractions in response to external forces. Utilizing stretch receptors, this system continuously monitors the positions of joints throughout the body.
Comprising nerves in the skin, muscles, joints, internal organs, and incorporating hearing, the Somatosensory System plays a crucial role in pilot awareness. The nerves in the body sense pressure differentials, allowing pilots to feel G-forces and pressures, such as inertia. The concept of "seat of the pants flying" originates from the feedback provided by the Somatosensory System.
Additionally, binaural hearing is highlighted as an essential component. Our ability to perceive sound direction contributes to situational awareness. The distinct sounds of an overspeeding propeller, air rushing against the airframe, or an abrupt engine failure are examples of how hearing aids pilots in determining their position relative to these auditory cues.
Spatial Disorientation training is essential for pilots to comprehend the human system's vulnerability to spatial disorientation. This practice emphasizes that judgments about aircraft attitude based on bodily sensations can often be misleading.
By fostering confidence in relying on flight instruments for accurate assessments of aircraft attitude, this training aims to reduce the frequency and severity of disorientation. It is crucial to note that pilots should refrain from attempting these maneuvers at low altitudes or without the guidance of an instructor pilot or an appropriate safety pilot.
Practicing controlled aircraft maneuvers for spatial disorientation is vital for pilots. It offers crucial insights into the limitations of the human sensory system during flight. Creating intentional illusions helps pilots recognize false perceptions, emphasizing the need to rely on flight instruments. This training enhances a pilot's ability to cope with unexpected situations, especially in low-visibility conditions, ultimately improving awareness and decision-making for safe flight operations.
Practicing controlled aircraft maneuvers to induce spatial disorientation is crucial for pilots as it provides valuable insights into the limitations and vulnerabilities of the human sensory system during flight. The intentional creation of illusions through these maneuvers underscores the potential for false perceptions and the challenges of maintaining accurate spatial awareness. Experiencing disorientation in a controlled environment helps pilots recognize the sensations associated with spatial illusions, fostering a deeper understanding of the need to rely on flight instruments. This practice enhances a pilot's ability to cope with unexpected situations, especially in low-visibility or instrument meteorological conditions, where visual references are limited. Ultimately, the importance of such training lies in improving a pilot's awareness, proficiency, and decision-making skills to ensure safe and effective flight operations.
Vestibular illusions in aviation safety involve misperceptions of aircraft motion due to conflicts between inner ear sensations and visual cues. Pilots must recognize and understand these illusions to prevent spatial disorientation and make safe decisions, especially in situations with limited or compromised visual references.
Visual illusions pose a significant threat to pilots as they heavily rely on their eyes for accurate information. Among these illusions, false horizon and autokinesis specifically impact the visual system. False horizon can occur due to factors like sloping cloud formations or obscured horizons, leading pilots to misinterpret their aircraft's attitude. Autokinesis, observed during night flying, involves a stationary light appearing to move after prolonged focus, potentially causing pilots to lose control. Vigilance, proper training, and reliance on instruments become crucial in mitigating the risks associated with these visual illusions for overall aviation safety.
Vision plays a crucial role in ensuring safe flight; however, optical illusions can be introduced by different terrain features and atmospheric conditions, especially during the landing phase. As pilots shift from relying on instruments to visual cues for landing at the conclusion of an instrument approach, it becomes vital for them to recognize and address potential issues related to these illusions. The following are major illusions that can contribute to landing errors and should be understood by pilots for safe and effective landings.
An upsloping runway or terrain, or a combination of both, can create the illusion that the aircraft is at a higher altitude than its actual position. If the pilot fails to recognize this illusion, it may result in a lower approach. Conversely, downsloping runways and approach terrain can induce the opposite effect, potentially leading the pilot to fly a higher approach. Awareness of these slope-related illusions is vital for maintaining accurate altitude assessment during approach and landing.
Vision plays a crucial role in ensuring safe flight; however, optical illusions can be introduced by different terrain features and atmospheric conditions, especially during the landing phase. As pilots shift from relying on instruments to visual cues for landing at the conclusion of an instrument approach, it becomes vital for them to recognize and address potential issues related to these illusions. The following are major illusions that can contribute to landing errors and should be understood by pilots for safe and effective landings.
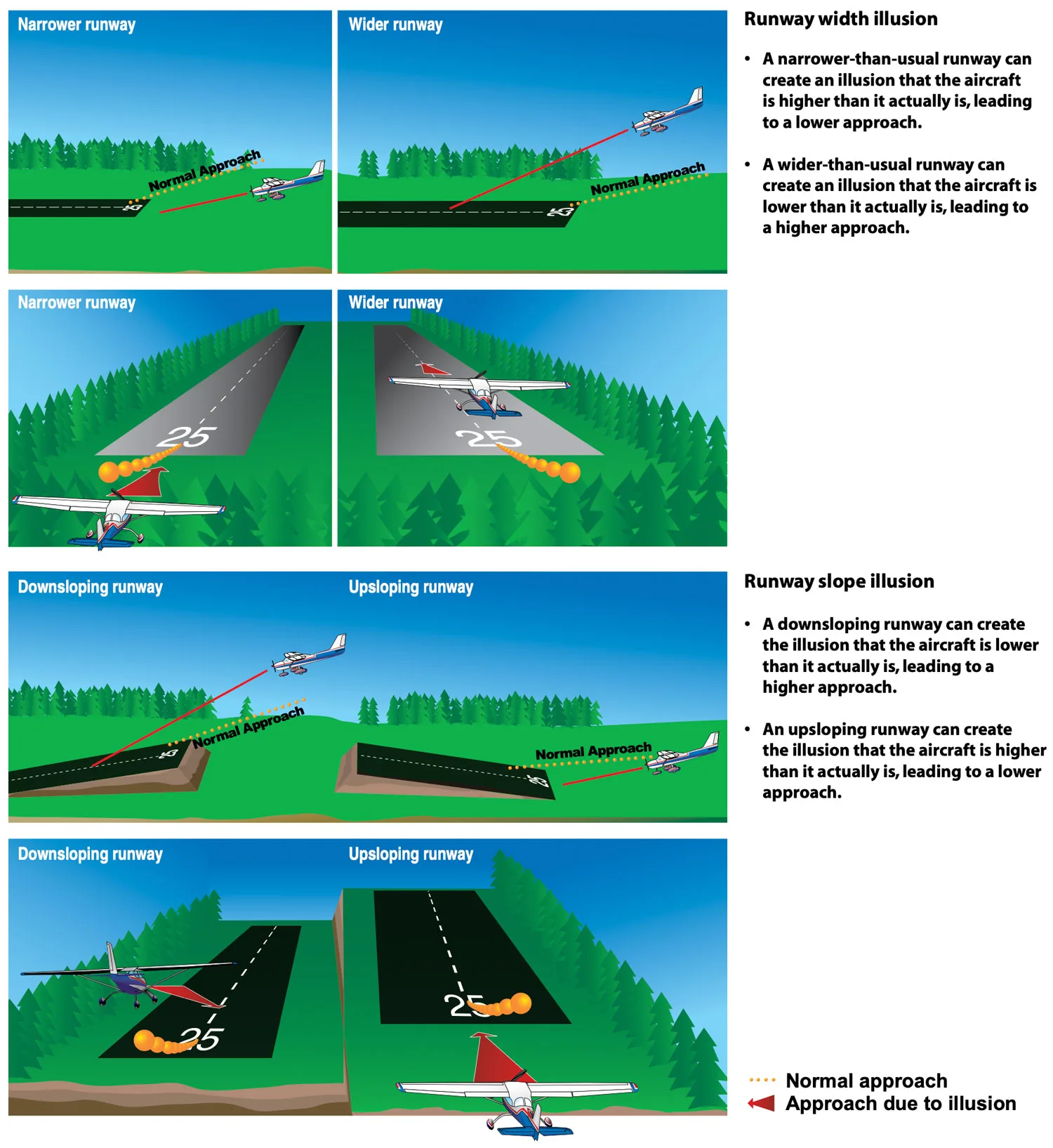
To prevent potential landing hazards resulting from optical illusions, pilots can take several proactive measures:
Anticipate: It's crucial to anticipate the possibility of visual illusions, especially during approaches to unfamiliar airports, particularly at night or in adverse weather conditions. Consulting airport diagrams and the Chart Supplement U.S. for details on runway slope, terrain, and lighting is essential.
Reference Altimeter: Regularly referencing the altimeter is a fundamental practice.
Aerial Inspection: Whenever possible, conducting aerial visual inspections of unfamiliar airports before landing can provide valuable insights.
Use Visual Aids: For maintaining a visual reference, pilots are advised to use Visual Approach Slope Indicator (VASI) or Precision Approach Path Indicator (PAPI) systems.
Electronic Glideslopes: Electronic glideslopes and visual descent points (VDP) on nonprecision instrument approach charts also contribute to safer landings.
Remain Vigilant: Pilots should remain vigilant during emergencies or distracting activities, recognizing that maintaining proficiency in landing procedures is crucial.
This proactive approach is vital, given that visual and sensory illusions are commonly cited factors contributing to fatal aviation accidents. Specific examples include sloping cloud formations, obscured horizons, and various atmospheric conditions that can create misperceptions during landings.
Flying with any sinus infection or ear blockage can pose serious health risks, potentially leading to the rupture of the eardrum. Understanding Boyle's Law is essential in grasping this concept, as it states that the pressure of a gas decreases as its volume increases. During climbs and descents, the free gas in various body cavities expands due to the pressure difference between the external and internal air.
If the release of this expanded gas is obstructed, pressure accumulates within the cavity, causing pain. This trapped gas expansion results in ear and sinus pain, accompanied by a temporary reduction in hearing ability. It is crucial to avoid flying with such conditions to prevent these severe health consequences.
The Eustachian Tube is responsible for equalizing pressure between the middle ear and the external environment. Normally closed, it opens during actions like chewing, yawning, or swallowing to maintain pressure equilibrium.
During a climb, the middle ear air pressure can exceed that of the external ear canal, causing the eardrum to bulge outward. Conversely, during a descent, the middle ear cavity, initially equalized at a higher altitude, is now at a lower pressure compared to the increasing pressure in the external ear canal. This results in a higher external pressure, causing the eardrum to bulge inward. Relieving this condition can be challenging, as the partial vacuum tends to constrict the walls of the Eustachian tube.
During ascent and descent, the sinuses equalize with the aircraft cabin pressure through small openings connecting them to the nasal passages. Conditions like a cold, sinusitis, or nasal allergies can cause congestion around these openings, impeding equalization and potentially leading to a "sinus block," commonly occurring during descent.
This blockage can affect frontal sinuses above the eyebrows or maxillary sinuses in the upper cheeks, causing intense pain and even bloody mucus discharge. Prevention involves avoiding flight with upper respiratory infections or nasal allergies, as decongestants may not provide sufficient protection.
Oral decongestants, with performance-impairing side effects, should be used cautiously, and persistent issues require consultation with a physician.
Dive into the world of gases with Hank in this Crash Course Chemistry episode. Discover how the Ideal Gas Law, crafted by brilliant minds (excluding Robert Boyle), demystifies pressure, volume, temperature, and moles. Unravel the complexities of gas behavior in a concise exploration of chemistry and physics.
The Valsalva Maneuver is employed to clear ear blockage.
This procedure involves forcing air through the Eustachian tube into the middle ear.
It may not be possible to equalize pressure in the ears if a pilot has a cold, an ear infection, or a sore throat.
If a sinus block occurs, it can produce excruciating pain over the sinus area or make upper teeth ache. Bloody mucus may discharge from the nasal passages.
Prevention is key; avoid flying with an upper respiratory infection or nasal allergic condition.
Decongestant sprays or drops may not provide adequate protection, and oral decongestants have potential side effects that can impair pilot performance.
If a sinus block does not clear shortly after landing, consulting a physician is recommended.
Motion sickness, or "vestibular disorientation," is a common challenge for pilots, resulting from a disconnect between visual and vestibular stimuli. This leads to conflicting messages to the brain about the body's motion, causing symptoms like nausea, dizziness, sweating, and, in severe cases, vomiting.
This condition is intricately linked to the interplay between visual cues, the inner ear's vestibular system, and other sensory inputs. When these signals conflict, it can result in the typical symptoms associated with motion sickness.
As a pilot, recognizing these early signs is crucial for effective management. Proactive measures, such as maintaining focus on the horizon, avoiding excessive head movements, and considering motion sickness glasses or medication under aviation medical guidance, can contribute to a more comfortable and safe flying experience.
As a pilot, being attuned to the early signs of motion sickness is essential for prompt intervention. The symptoms of motion sickness include nausea, dizziness, sweating, and, in severe cases, vomiting. Keep an eye out for any sensations of imbalance or discomfort. If you notice these symptoms, take immediate action to address the situation. Early recognition allows for more effective management and ensures the safety and well-being of both the pilot and passengers.
Motion sickness is a common challenge for pilots, but there are measures to help mitigate its effects. By paying attention to these preventive measures, you can significantly reduce the likelihood of experiencing motion sickness during flights. Here's a simplified guide:
Prioritize Overall Health: Ensure you are well-rested and hydrated before a flight to minimize susceptibility.
Consider Flight Factors: During flight planning, factor in weather, turbulence, and maneuver complexity to anticipate triggers.
Ventilation Matters: Maintain adequate cockpit ventilation for a more comfortable environment.
Smooth Control Inputs: Implement gentle and smooth control inputs, avoiding abrupt maneuvers to minimize conflicting sensory signals.
Regular Flight Training: Conduct regular flight training to enhance your tolerance to motion variations.
Dealing with motion sickness symptoms during a flight requires quick and appropriate action for a safe and comfortable journey. Address motion sickness promptly by prioritizing these strategies for yourself and your passengers to ensure a smoother flight experience. Here are some practical tips:
Focus on the Horizon: Adjust your focus to the horizon, providing a stable visual reference.
Minimize Head Movements: Avoid activities that could worsen the disconnect between visual and vestibular stimuli.
Ventilation is Key: Open fresh air vents to improve airflow and reduce the impact of cabin odors.
Controlled Breathing: Engage in controlled breathing techniques to ease discomfort.
Stay Hydrated: Maintain hydration, as it can contribute to alleviating symptoms.
Carbon Monoxide (CO), a colorless and odorless gas, poses a significant threat in aviation, primarily originating from combustion engines. Its lethal nature stems from its remarkable ability to bind to hemoglobin in the blood—200 times more effectively than oxygen (O2). This binding prevents hemoglobin from efficiently transporting oxygen to the body's cells, leading to a potential life-threatening situation.
What makes CO particularly insidious is its prolonged presence; it can take up to 48 hours to be completely removed from the body. In the aviation context, there's an additional risk of CO entering the aircraft through heating ducts, especially if there's a crack in the exhaust manifold. This underlines the importance of meticulous maintenance practices and regular inspections to detect and rectify potential sources of CO leakage.
Pilots and aviation personnel must be acutely aware of these risks, emphasizing the need for comprehensive pre-flight checks and monitoring of the aircraft's heating and ventilation systems. Understanding the dynamics of CO poisoning is fundamental in ensuring the safety and well-being of everyone on board.
Embark on a gripping narrative in this NTSB video as Dan Bass shares his harrowing encounter with CO Poisoning during a flight. His firsthand experience serves as a stark testament to the grave dangers posed by CO Poisoning, underscoring that it's not just a matter of safety but one of life and death.
Common Symptoms
Symptoms for CO Poisoning are Headaches, dizziness, weakness, nausea, vomiting, chest pain, loss of muscular power, blurred vision, and confusion. Recognizing these signs early on is crucial for effective management.
Common Preventive Measures
Preventing CO poisoning is crucial for aviation safety. Regularly inspect and maintain the aircraft's exhaust system to identify and fix leaks promptly. Install and maintain CO detectors in the cockpit.
During pre-flight checks, be attentive to any unusual odors or symptoms. Educate passengers on the importance of reporting any symptoms promptly. Implement thorough pre-flight briefings regarding the dangers of CO poisoning and the significance of maintaining awareness during the flight.
Treatment Strategies:
If a pilot suspects CO poisoning, the first step is to use supplemental oxygen if available. Declare an emergency and communicate with air traffic control to get priority handling for landing. Land as soon as possible, as the treatment for CO poisoning is the administration of 100% oxygen.
Seek immediate medical attention on the ground to ensure a comprehensive evaluation and appropriate medical care. Early recognition, prevention, and swift action are critical in managing CO poisoning for pilots.
In aviation, adherence to supplemental oxygen requirements is essential for the safety and well-being of both the flight crew and passengers, as outlined in FAR §91.211. The Federal Aviation Administration (FAA) mandates these requirements to ensure proper oxygen levels are maintained at different altitudes. Here's a breakdown:
Above 12,500 Feet: After 30 minutes at this altitude, supplemental oxygen is required for the flight crew.
Above 14,000 Feet: Supplemental oxygen is mandated for the flight crew at all times.
Above 15,000 Feet: At this altitude, supplemental oxygen is not only required for the flight crew but must also be provided to passengers.
These regulations are designed to mitigate the risks associated with decreased oxygen levels at higher altitudes, safeguarding the health and performance of those on board. Pilots must be well-versed in these requirements to ensure compliance and prioritize the safety of the flight.
Stress, a potential precursor to serious health issues, manifests in three distinct types, each posing unique challenges. Left untreated, these stressors can escalate into critical health situations. The impact of stress is evident in heightened heart rate, accelerated respiration, increased blood pressure, and intensified perspiration. Recognizing and addressing these three types of stress is essential for maintaining overall well-being and preventing the escalation of health risks.
Physical symptoms of stress encompass a range of discomforts, such as low energy, headaches, and upset stomach, which may manifest as diarrhea or constipation. Nausea is also a common response to heightened stress levels. Additionally, individuals experiencing stress often report aches, pains, and muscle tension. Recognizing and addressing these symptoms is crucial for overall well-being, especially in contexts where heightened stress, such as in aviation, can impact performance and safety.
Physiological or biological stress refers to an organism's response to a stressor, which can be an environmental condition or any factor that challenges the organism. Stress, in this context, is the body's natural way of reacting to such challenges. Understanding the physiological aspects of stress is vital, particularly in aviation, where pilots encounter various environmental factors that can act as stressors, influencing their physical and mental well-being.
Psychosocial stress arises from an individual's mental interpretation of events and their perceived ability to cope with them. This form of stress is deeply connected to our understanding and response to social threats, whether real or imagined. In aviation, psychosocial stress can manifest when pilots face challenging situations, and their mental and emotional well-being plays a crucial role in decision-making and overall safety. Recognizing and managing psychosocial stress is essential for maintaining optimal pilot performance and ensuring a safe flight environment.
Fatigue in aviation arises from inadequate sleep and excessive physical or mental strain, often contributing to pilot error. The lack of sufficient rest can compromise cognitive functions and decision-making, posing significant risks to aviation safety. Identifying signs of fatigue and adopting strategies for prevention are vital for maintaining pilot well-being and competence. Addressing fatigue is essential to create a safe and effective operational environment in aviation.
Understanding and addressing these specific types of fatigue in the context of aviation is essential for pilots to maintain optimal performance, ensure safety, and mitigate the risks associated with the demanding nature of their profession.
Acute fatigue, often known as short-term fatigue, is a common challenge for pilots during brief periods of intense mental or physical exertion. This can occur during demanding phases of flight, like critical decision-making moments or navigating challenging weather conditions.
Acute fatigue can lead to a temporary decline in cognitive performance, attention, and reaction times. Recognizing signs such as increased irritability or reduced alertness is crucial for pilots. In these situations, prioritizing immediate rest and recovery is essential to mitigate the impact on flight safety.
Chronic fatigue, or long-term fatigue, is a sustained and persistent condition that can significantly impact a pilot's overall well-being and flight performance. It often arises from continuous exposure to stress, insufficient rest, or an irregular sleep pattern over an extended period. Pilots experiencing chronic fatigue may encounter symptoms such as mental fog, difficulty concentrating, and reduced decision-making capabilities.
To address chronic fatigue, it is vital for pilots to establish healthy sleep routines, maintain a balanced lifestyle, and seek professional guidance if necessary. Prioritizing regular breaks, proper nutrition, and sufficient sleep are crucial measures to manage and prevent the adverse effects of chronic fatigue in aviation.
Treating fatigue as a pilot involves a multifaceted approach to ensure optimal performance and safety. By following these measures, pilots can maintain peak performance levels and ensure the highest standards of safety during flight operations. Here are key steps:
Prioritize Adequate Sleep: Ensure consistent and sufficient sleep patterns, allowing for recovery time between flights.
Manage Workload: Avoid overcommitting to extended duty hours and take regular breaks during flights to combat mental and physical fatigue.
Healthy Lifestyle Habits: Incorporate regular exercise and maintain a balanced diet for overall well-being.
Supportive Work Environment: Foster an atmosphere that encourages open communication about fatigue-related concerns.
Self-Awareness: Stay attuned to personal fatigue indicators and recognize when rest is necessary.
Dehydration, a common concern for pilots, can significantly impact both physical and cognitive performance. This condition arises when the body loses more free water than it takes in, a situation exacerbated by various factors in the aviation environment.
Pilots may be exposed to high-temperature flight decks, leading to increased perspiration and potential fluid loss. Additionally, the consumption of diuretics such as coffee, tea, and alcohol can contribute to the body's water imbalance. Prolonged flights at high altitudes, with lower humidity levels, also increase the risk of dehydration.
Stay Hydrated: Prioritize regular water intake before, during, and after flights.
Limit Diuretics: Consume coffee, tea, and alcohol in moderation to avoid excess fluid loss.
Monitor Environment: Be vigilant in high-temperature conditions to prevent dehydration.
Dehydration: Drink water or electrolyte-rich fluids promptly to restore fluid balance.
Rest: Allow time for recovery and avoid engaging in strenuous activities.
Seek Medical Attention: In severe cases, consult a healthcare professional for proper evaluation and guidance.
Quality sleep is foundational for pilot health, and its importance extends crucially to aviation safety. The demanding nature of piloting necessitates optimal cognitive function, alertness, and precise decision-making – all of which are intricately tied to sleep quality. Fatigue, often a result of inadequate sleep, poses a substantial risk to pilots' well-being and, subsequently, to the safety of air travel.
Fatigue manifests as a complex interplay of physical and mental exhaustion in pilots. Prolonged wakefulness, irregular sleep patterns, and extended duty hours contribute to this fatigue, potentially compromising a pilot's ability to perform optimally. This fatigue-induced impairment can mimic the effects of alcohol, impacting coordination, reaction times, and situational awareness.
Recognizing the critical link between fatigue and safety, the aviation industry enforces stringent regulations. Duty-time limitations and rest requirements are in place to mitigate the risks associated with fatigue-induced impairments. Understanding that fatigued pilots are more susceptible to errors and lapses in judgment, these regulations uphold the highest standards of safety in air travel.
For pilots, prioritizing healthy sleep habits is not just a personal wellness consideration; it's a professional responsibility that directly influences safety. Adequate sleep is paramount for maintaining peak cognitive function, vigilance, and overall health. By fostering a culture of sleep awareness and prioritizing healthy sleep practices, pilots actively contribute to their own well-being and play a vital role in ensuring the safety of the skies they navigate.
Homeostatic Influence: The body's call for sleep arises from the accumulation of certain substances during extended wakefulness. As extracellular adenosine levels elevate, the irresistible urge to sleep ensues.
Staying Awake? Coffee to the Rescue: Combat the drowsy effects by leveraging the power of coffee, which blocks adenosine receptors, offering a temporary reprieve.
Circadian Rhythm: At the heart of the 24-hour circadian rhythm lies the main sleep drive. Cells within the suprachiasmatic nucleus fire in a meticulously orchestrated 24-hour cycle, reset daily by factors such as light exposure, work and rest schedules, and regular social interaction.
Circadian Clock Realities: The circadian clock exhibits an inability to promptly adapt to new environmental times or changes in duty/rest schedules, underscoring the challenges pilots may face in aligning their internal clock with dynamic operational demands.
For pilots, navigating these influences is a strategic imperative. Recognizing the interplay of homeostasis and circadian rhythm equips aviators with insights to optimize sleep, promoting heightened alertness for safe and effective flight operations.
Sleep cycles are intricate processes that pilots must comprehend for optimal well-being and performance. The two main categories are Non-Rapid Eye Movement (NREM) and Rapid Eye Movement (REM). These cycles consist of various stages, each playing a crucial role in physiological and cognitive restoration.
In the NREM phase, pilots traverse through different stages, each with distinct characteristics. Stage 1 (N1) marks the transition from wakefulness to sleep, lasting only a few minutes. Stage 2 (N2) is where true sleep begins, slightly deeper than N1 and lasting around 20 minutes.
The pinnacle is Stage 3 (N3), characterized by delta waves, vital for physical restoration. This stage facilitates repair and regeneration of tissues, muscle and bone strengthening, and provides a significant boost to the immune system.
The REM stage is where brain activity intensifies. During this stage, the heart rate and breathing become inconsistent, rapid eye movements occur, and skeletal muscles are temporarily paralyzed in short increments throughout the night. It is in REM sleep where pilots experience the most intense dreaming. This stage is not only crucial for mental recuperation but also facilitates memory storage and retention, organization, and reorganization, as well as new learning and performance.
Understanding the architecture of sleep is like navigating through a flight plan. A full sleep cycle lasts around 90-110 minutes, with multiple cycles occurring throughout the night. The transitions between NREM and REM stages constitute a complete sleep cycle. Pilots need to recognize this pattern to optimize their rest effectively.
Sleep is not merely a physiological necessity; it is a fundamental component of pilot performance. Cognitive restoration occurs during NREM and REM, ensuring pilots are mentally sharp. REM sleep plays a pivotal role in memory storage and learning, essential for acquiring and retaining the intricate knowledge required in aviation. Quality sleep directly contributes to optimal performance in the cockpit, enhancing decision-making and responsiveness.
Pilots can take proactive steps to optimize their sleep. Maintaining a consistent sleep schedule aligned with regular duty hours is paramount. Creating a comfortable sleep environment with minimal disturbances enhances sleep quality. Prioritizing sleep hygiene involves developing bedtime rituals for better sleep quality. Recognizing individual sleep needs and listening to the body's natural requirements ensure that pilots get the rest they need to perform at their best.
This video decodes the secrets of circadian rhythm. Learn how to sync your internal clock with the demands of aviation, optimizing sleep and enhancing alertness. Elevate your performance for safer and more efficient flights.
Pilots under the influence of drugs or alcohol can experience severe impairment, jeopardizing both their safety and that of others on board. Substance use can lead to compromised cognitive functions, impaired decision-making, slowed reaction times, and diminished situational awareness—critical elements for safe flying.
From a legal perspective, operating an aircraft while under the influence of drugs or alcohol is a serious offense. Aside from the immediate threat to safety, it can result in severe legal consequences. Violation of aviation regulations, such as 14 CFR, can lead to the suspension or revocation of a pilot's license. Legal penalties may include fines, imprisonment, and a permanent ban on flying.
Pilots must prioritize their well-being and the safety of passengers by adhering to strict regulations regarding substance use. Compliance with these rules is not only crucial for maintaining a pilot's professional standing but, more importantly, for ensuring the highest standards of safety within the aviation industry.
Alcohol remains a significant hazard for both general aviation and airline pilots. The FAA mandates an 8-hour waiting period after consuming alcohol before a pilot can operate an aircraft. Moreover, many air carriers impose a more stringent requirement of a 12-hour waiting period. The maximum allowable limit for alcohol in a pilot's system is 0.04% BAC, which is half the legal limit for operating a motor vehicle in the United States.
Operating an aircraft with any amount of alcohol in the system can result in severe consequences for a pilot's career, especially in the context of airline operations. It's crucial to note that 0.04% BAC represents the limit, not the permissible total amount. Flight crews may find themselves subjected to a FAA-mandated DOT drug test following a night of excessive alcohol consumption, leading to potential career-ending repercussions, disregarding both FAA guidance and air carrier company policy.
For pilots, the phenomenon of Decompression Sickness (DCS) is a crucial consideration when operating at different altitudes. Exposure to lower pressures can cause nitrogen, normally dissolved in body fluids and tissues, to form bubbles as pressure decreases. These bubbles can lead to diverse signs and symptoms, impacting a pilot's well-being and performance.
Henry’s law plays a pivotal role in this process, emphasizing that the amount of dissolved gas in bodily fluids is directly linked to the partial pressure of that gas in equilibrium with the liquid. This understanding is particularly relevant for pilots who experience varying altitudes during flights.
It's essential for aviators to be aware that signs of DCS may not immediately manifest; symptoms could appear up to 60 minutes after exposure, and in certain cases, even after 24 hours. Pilots must prioritize safety measures and adhere to established protocols to minimize the risk of DCS, ensuring their well-being and the safety of their flights.
After engaging in scuba diving activities, pilots need to observe specific waiting periods to minimize DCS risks. For dives at or below a Pressure Altitude (PALT) of 8,000 feet, a 12-hour wait is recommended following a non-decompression stop dive. If the dive involves a controlled ascent (decompression-stop dive) or is at or above a PALT of 8,000 feet, a full 24-hour wait is necessary before resuming flight.
This waiting period is crucial for both pilots and medical professionals, aligning aviation safety with medical best practices. Pilots must be vigilant in adhering to these guidelines to ensure their well-being and mitigate the potential consequences of DCS during flight operations.